An antibiotic stewardship program in general surgery leads to better antibiotic use and cost savings
Author(s):
Erica Secchettin; Salvatore Paiella; Matteo De Pastena; Elena Carrara; Anna Maria Azzini; Laura Addari; Giuseppe Malleo; Evelina Tacconelli; Claudio Bassi; Roberto Salvia
Background:
Antimicrobial resistance is a worldwide growing public healthcare problem. The WHO tackles this by promoting judicious antibiotic use. Recently, broad-spectrum WHO-defined “Watch” antibiotics have been surprisingly proposed in pancreatic surgery. Antimicrobial stewardship programs (ASP) are effective in improving antibiotic use. Using an interrupted time series analysis, the ability of a prospective ASP in pancreatic surgery to evaluate the changes in antibiotics consumption and cost savings before and after the program implementation was assessed.
Hypothesis:
An ASP program in general surgery leads to better antibiotic use and cost savings.
Methods:
Data were derived from a single center involved in a multicenter ASP, the Pancreatic Surgery Unit of the University of Verona. The ASP pivoted on tailored antibiotic prophylaxis based on the results of a preoperative rectal swab. Pancreatic surgeries only were included. The study period went from 2015 to 2022. Two time periods were compared, pre-ASP (2015-2018) and post-ASP implementation (2019-2022). Drug consumption of systemic antibiotics (presented as anatomical therapeutic chemical – ATC-J01/defined daily doses – DDD – and normalized per 1000 patients-days (PDs), the trend of “Access” and “Watch” (according to WHO definitions) antibiotics use, and cost savings were evaluated. The two phases were compared.
Results:
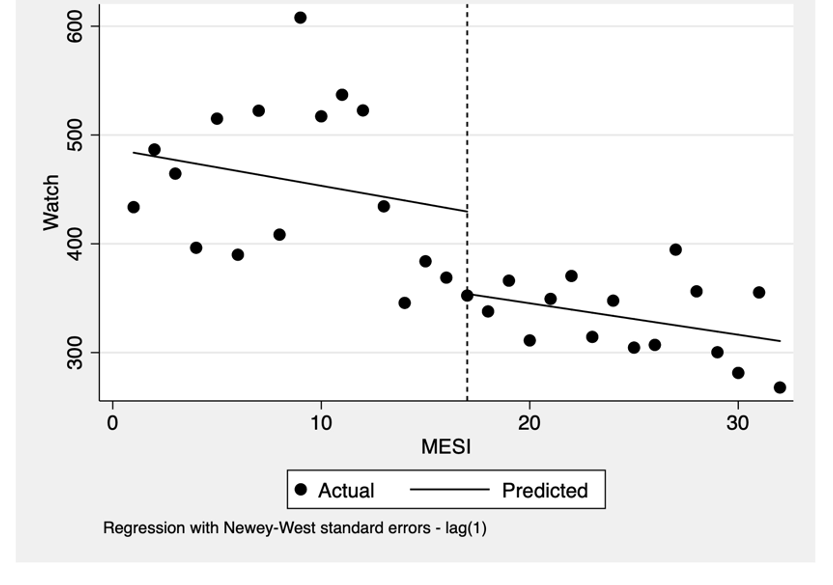
The ASP was associated with a statistically significant reduction in the use of “Watch” antibiotics (-2.89, 95%CI [-5.55 – – 0.23], p= 0.0341, Figure 1), followed by non-statistically significant increased use of “Access” antibiotics (3.48, 95%CI [- 4.93 – 11.89], p= 0.404), measured in DDD/1000 PDs. The ASP also produced an overall monthly cost reduction despite not being statistically significant (-241.62€; p= 0.523). The total cost savings was 24746,40€. The “Watch” antibiotics cost was reduced by 22292,03€, whereas the “Access” ones increased by 5291,60€.
Conclusions:
An ASP in general surgery produces important changes in antibiotic use, with a reduction in “Watch” antibiotics prescription, according to the WHO principles of appropriate and judicious use of antibiotics. Besides the clinical benefits, such as surgical site infection and major complication reduction, an ASP may also have positive pharmacoeconomic effects.
