An Actionable Risk Model for the Development of Surgical Site Infection Following Emergency Surgery
Author(s):
Ari Wes; Joseph Fernandez-Moure; Lewis Kaplan; John Fischer
Background:
Surgical site infections (SSI) increase mortality and the economic burden associated with emergency surgery (ES). A reliable and sensitive scoring system to predict SSI can help guide clinician assessment and patient counseling of post-operative SSI risk.
Hypothesis:
We hypothesized that after quantifying the ES post-op SSI incidence, readily abstractable variables can be used to develop an actionable risk stratification scheme.
Methods:
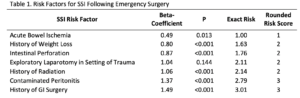
We retrospectively reviewed all patients who underwent ES operations at an urban academic hospital system (2005-2013). Comorbidities and operative characteristics were abstracted from the electronic health record (EHR) with a primary outcome of post-op SSI. SSI risk was calculated using logistic regression modeling and validated using bootstrapping techniques. Beta (β) coefficients were calculated to correlate risk. A simplified clinical risk assessment tool, the emergency surgery infection risk score (ESIRS) was derived by assigning point values to the rounded β-coefficients.
Results:
4,783 patients with a 13.2% incidence of post-op SSI were identified. The strongest risk factors associated with SSI included acute intestinal ischemia, weight loss, intestinal perforation, trauma related laparotomy, radiation exposure, previous gastrointestinal surgery, and contaminated peritonitis (Table 1). The assessment tool defined three patient groups based on SSI risk. Post-op SSI incidence in high risk patients (34%; ESIRS score= 6-10) exceeded that of medium (11.1%; ESIRS score =3-5) and low-risk patients (1.5%; ESIRS score =1-2) (C-statistic=0.802). Patients with a risk score > 10 points evidenced the highest post-op SSI risk (71.9%).
Conclusions:
Preoperative identification of ES patient risk for post-op SSI may inform pre-operative patient counseling and operative planning if the proposed procedure includes medical device implantation. A clinically relevant 7-factor risk stratification model such as this empirically derived ESIRS may be suitable to incorporate into the EHR as a decision-support tool.
An Actionable Risk Model for the Development of Surgical Site Infection Following Emergency Surgery
Author(s):
Christopher Towe, Nathaly Llore, Nathalie Hirsch, Jessica Donington, Harvey Pass, Vanessa Ho, NYU Langone Medical Center
Background: Empyema can result as a complication of bacterial pneumonia or thoracic surgery procedures with mortality as high as 15%. Empyema pathogens are poorly described in the modern era. Greater understanding of common pathogens and risk factors is required to improve empiric treatment. The primary aim of this study is to describe the microbiology of empyema in the modern era.
Hypothesis: We hypothesize that parapneumonic empyema (PNE) and post-surgical empyema (PSE) will be clinically and microbiologically distinct.
Methods: All patients with positive pleural cultures between 4/2007 and 6/2012 were identified from microbiological records. Patient demographics, clinical course and microbiological information were collected. Each acute empyema was classified as PNE or PSE and differences between groups were assessed using the Chi-square test.
Results: A total of 227 microorganisms from 28 genus classes were isolated from 125 patients (74 (64%) male, mean age 61). 120 (97%) required drainage and/or decortication, while 5 were treated with antibiotics alone. Common comorbidities included: a history of immunosuppression (29%), diabetes (19%), and renal disease (14%). Mortality was 15%. Half (47.7%) of the index cultures were polymicrobial. 152 isolates (67%) were gram positive, 56 (25%) were gram negative, 16 (7%) were fungal, and 3 (1%) were unclassified. Only 7% of isolates were obligate anaerobes. The most common organisms were Streptococcus spp (27%) and Staphylococcus spp (25%), followed by Enterococcus spp (9%), Candida (6%), and Pseudomonas (6%). Of 31 isolates of S. aureus, 14 (45%) were methicillin resistant. 29% of the infections were postoperative. Patients with PSE were less likely to have had a preceding pneumonia (28% vs 65%, p<0.05). Patients with PSE had a slightly higher incidence of gram-negative pathogens but this did not reach statistical significance (40% vs 26%, p=0.1). There was no difference in outcome between the PNE and PSE patients. Conclusions: A wide variety of pathogens were isolated from infected pleural cultures. The most common pathogens isolated were aerobes and gram positives. Polymicrobial infections were common. There was no significant difference in clinical course or pathogens isolated from parapneumonic and post-surgical empyema.
