Cross-Border Antibiotic Resistance Patterns in Trauma Patients
Author(s):
Allison Berndtson; Robin Bricker-Ford; Gabrielle Z. Madsen; Kevin Box; Todd Costantini; LeGrand Malany; Alan Smith; Raul Coimbra
Background:
Antibiotic resistant bacteria are a growing problem worldwide, with differences in regional resistance patterns driven by local variance in antibiotic stewardship. Resistant gram-negative organisms are increasingly prevalent in Latin America and account for a higher percentage of infections than in the United States (USA) or Canada. Hospitals along the US-Mexico border increasingly identify resistance, raising concern for transfer of drug resistant (DR) organisms across the border.
Hypothesis:
Patients transferred to a US trauma center after initial treatment by a healthcare facility in Mexico (MEX) will have a higher incidence of infections due to antibiotic-resistant organisms, including DR gram-negative bacteria.
Methods:
The registry of an ACS verified Level-1 trauma center was queried for all trauma admissions between March 1, 2011 and August 30, 2015. Patients were included if at least 1 culture was sent during the first 3 days of hospitalization, to avoid analysis of hospital-acquired bacteria. Patients were divided into two groups based upon injury location: inside the USA or in MEX. Cultures were reviewed to remove duplicate results and for confirmation of clinical infection.
Results:
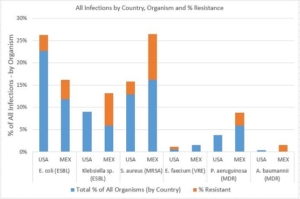
A total of 127 MEX and 1149 USA patients were analyzed. MEX patients were younger (45.5 vs 60.4 years), more likely to be male (68.5% vs 60.1%) and Hispanic (64.6% vs 32.3%), had a higher median ISS (21 vs. 10), and longer hospital lengths of stay (11.1 vs 5.5 days). MEX patients most commonly had respiratory infections (53.9%), while urinary tract infections were most common in USA patients (43.4%). MEX patients were more likely to have any type of resistant infection (26.5% vs 7.1% of all organisms grown, p<0.001). Resistance was more common in MEX patients with Klebsiella (55.6% ESBL vs 0%, p=0.01) or any gram negative infection (39.3% vs 10.4%, p=0.005). 15.0% of MEX organisms were untreatable by both piperacillin-tazobactam and vancomycin, our empiric regimen, as compared to 4.8% of USA organisms (p = 0.028).
Conclusions:
Antibiotic resistance is more common in patients initially treated in MEX healthcare facilities than those treated exclusively in the USA, despite close geographic proximity. MEX patients may require alternative empiric antibiotic regimens when presenting with infection. Global initiatives to improve antibiotic stewardship will be critical to limit the continued rise in drug-resistant infections.
